Sleep disordered breathing, snoring & OSA

Sleep apnoea and snoring occur due to airway obstruction during sleep, leading to breathing pauses or reduced airflow. This can cause fatigue, cognitive issues, and long-term health risks.
Sleep disordered breathing, snoring & OSA
Sleep apnoea and snoring is now thought to be one of the modern medical era pandemics. The incidence is increasing every year as our population becomes more obese and less active. Snoring is common in the general population. This is caused by vibration of soft tissues as it passes through the airway. It’s now estimated that approximately 20% of men and 5% of women aged 30-35 snore and by age 60 years, 60%of men and 40% of women are habitual snorers. A large percentage of snorers (literature suggests 30-50%) also have sleep apnoea.
Obstructive sleep apnoea is cessation (apnoea) or periodic reduction in airflow (hypopnoea meaning 50% reduction in airflow) during sleep due to obstructed airway. This is now being increasingly recognised by health professionals & patients. It is estimated that in the general population, 4% of males and 2% of females (aged 30 – 60) suffer from OSA. In the paediatric population, prevalence of obstructive sleep apnoea (OSA) is 3% (aged 0 – 15). The main symptoms of OSA include loud snoring in 80%, daytime sleepiness in 78%, cognitive deficits in 30%, road traffic accidents in 8%. They also have an increased prevalence of IHD, CVA and hypertension. It is well established that the risk factors for adult OSA’s include obesity (BMI > 30), male gender (twice as common), collar size > 17, mandibular hypoplasia (retronathia), hypothyroidism, nasal obstruction, evening alcohol consumption and cigarette smoking. Adeno-tonsillar hypertrophy is the commonest cause for paediatric OSA.
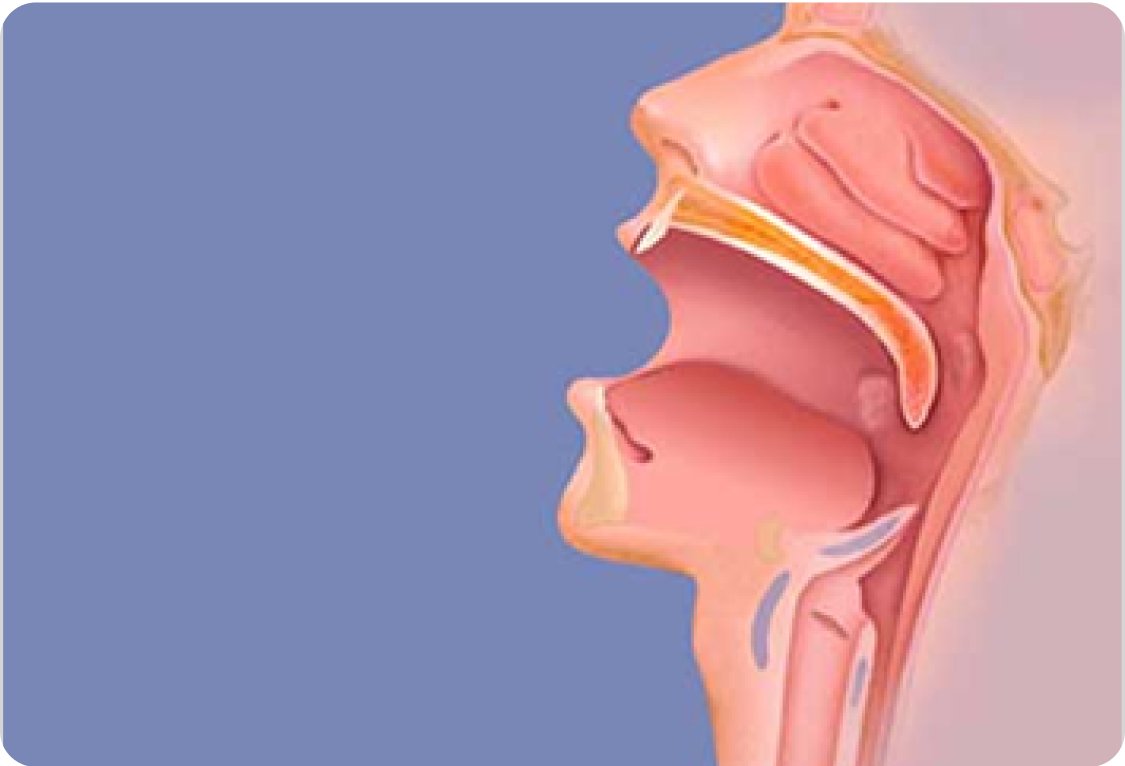
There has been increasing research and information in the literature regarding the pathophysiology of OSA and snoring in the last decade. In general, the obstruction in OSA and vibration in snoring is caused by collapse of the upper airway which can be at the level of the nose, nasopharynx, palate, tongue and larynx.
The postulated mechanisms are:
Insufficient muscle tone of palate, tongue, pharynx muscle and laryngeal muscle.
Obstructive lesions / soft tissue mass-like large tonsils, adenoids, tongue, long floppy soft palate, nasal polyps or septal deformity.
Mandibular or maxillary hyperplasia – retronathia, maxillary stunting.
Diagnosis
Patients and their partners usually give a good history of snoring and obstructive events. There are several symptoms and signs that may help you identify the patient who needs further investigations and treatment.
Some of the classic symptoms and signs of OSA are listed below and they include:
Loud snoring
Excessive day time sleepiness, causing depression, irritability, impaired job performance, auto accidents and hazardous driving
Abnormal muscular activity during sleep
Obesity
High blood pressure
Increased risk for heart attack, stroke, heart enlargement
Impaired intellectual performance
Morning headaches
Sexual impotence
Hyperactivity and anti social behaviour (children)
The commonest complaint in children is loud snoring, obstructive breathing with apnoeic spells, hyperactivity, anti-social behaviour, aggression, poor concentration etc. Parents of children with OSA often testify with video footage or tape recording to prove the events at night. Most patients will need a thorough examination of the upper airway including the nose, nasopharynx, soft palate, retro palatal area, tongue and larynx. Nasendoscopy may be required to see dynamic movement of structures and collapse of the obstructing airway.
Investigation
Approximately 30% to 50% of habitual snorers have OSA’s. It is difficult to identify the patient with OSA and its severity by history and examination alone. However, Epworth Sleepiness score >10, BMI>30, neck collar size >17 and >16 in females are additional information which may indicate patient has OSA’s. The gold standard in investigation is a diagnostic Polysomnography (PSG). There are several types of PSG testing however ambulatory monitoring of oxygen saturation, heart rate and nasal airflow measurement can be a useful screening tool. In children PSG is recommended but is expensive and labour intensive. Pulse oximetry studies can be used as a screening tool.
Treatment
Treatment options depend on each individual patient and their severity of symptoms. Dr Murali Mahadevan will guide you toward appropriate treatment.
Non Surgical Options
Oral mandibular advancement prosthesis: this appliance can draw the mandible (jaw) forward and increase the size of the oropharyngeal airway. Many patients cannot tolerate this at night mainly because of jaw pain, temporomandibular discomfort and dribbling of saliva.
Nasal Splints and Sparys: these enlarge the nasal passages will only work if nasal valve is blocked. This does not help if there are multiple obstructive sites at night when patient is lying supine.
Shoulder pillows / ball: these pervert from patient rolling on their back and has limited use in most snorers.
Weight loss and Exercise: this will help over weight patients with BMI over 40. But snoring and OSA still can occur in slim individuals.
Continuous Positive Airways Pressure CPAP: using a face mask or nasal prongs continuous pressure of air / oxygen is delivered to the patient during time of sleep via a machine. This is very effective in sleep apnoea and has a reported benefit in 65-70% patients. However about 50% of the patients cannot tolerate this treatment as along term option or can not tolerate for 6-8 hours at night. The machine costs around NZ$3500-5000.
Minimally Invasive Surgery
Septoplasty: correction of deviated nasal septum and reduction of enlarged inferior turbinates can improve airway. Surgery is a day surgical procedure and has the risks associated with General anaesthetic and bleeding. This does not help patients with multi level collapse of the airway.
Tonsillectomy: if the tonsils are enlarged and this can obstruct the airway. Tonsillectomy can improve the obstruction. Traditional tonsillectomy is painful and has the risk of bleeding. Coabalation tonsillotomy is less painful and has a risk of bleeding at the rate of 3%. Again this does not address other collapsing areas in the airway.
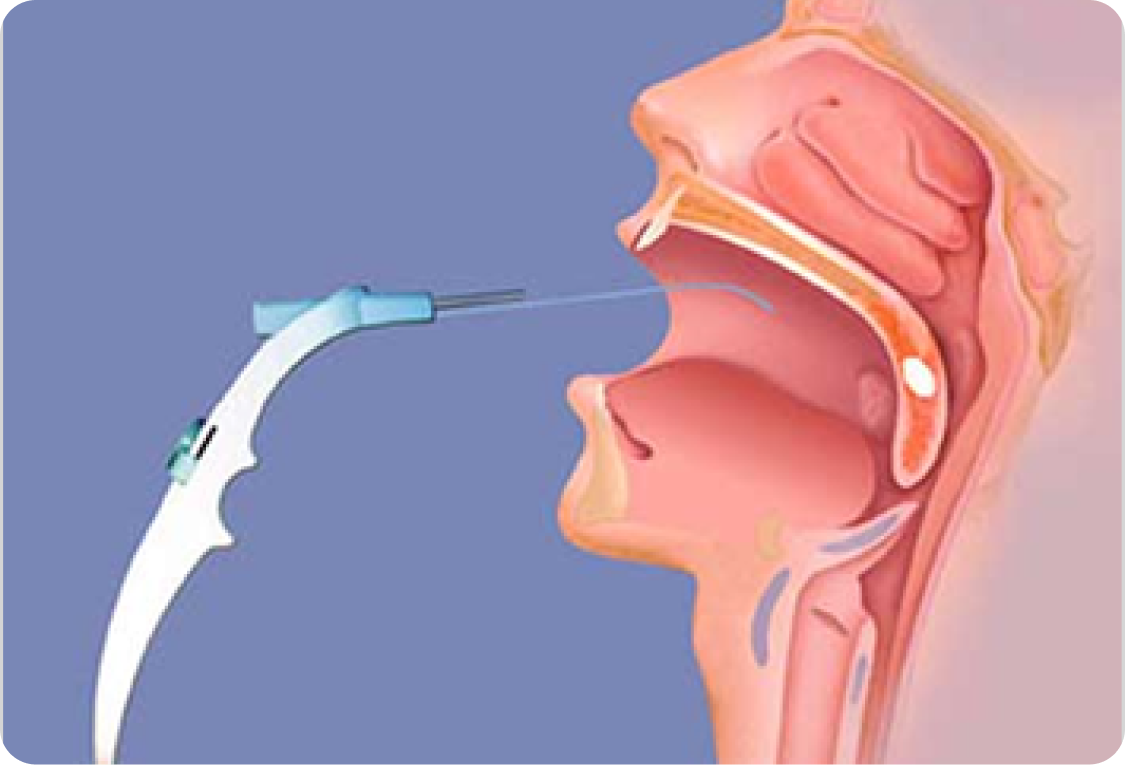
Injection Snoroplasty: injection of sclerosant to soft palate is an effective local anaesthetic procedure for most snorers. Injection of sclerosant Sodium Tertradycel sulphate 3% solution 2mls is injected to 5 different sites. This enables scar tissue to be formed in the soft palate muscle hence stiffens the tissue. Repeated injections can be given to enhance the effect. Day surgical local anaesthetic procedure and back to work in 2 days. Healing takes 1 week but full effect may take 6-8 weeks.
Somnoplasty: this is done as a local or general anaesthetic procedure with local anaesthetic spray and injection of local anaesthetic. Procedure is aimed at delivering approximately 600J of thermal energy at 50-60 degrees Celsius to the soft palate muscle. The procedure takes approximately 30 mins and done as a day procedure. Most patients have minimal pain which is well controlled with Paracetamol. There will be some swelling and discomfort for 3-5 days and most patients return to work in 3 days. The effects of the procedure take 4-6 weeks by tissue scar formation within the soft palate muscle. Success rate is approximately 70%.
Surgery for bad snorers and sleep apnoea
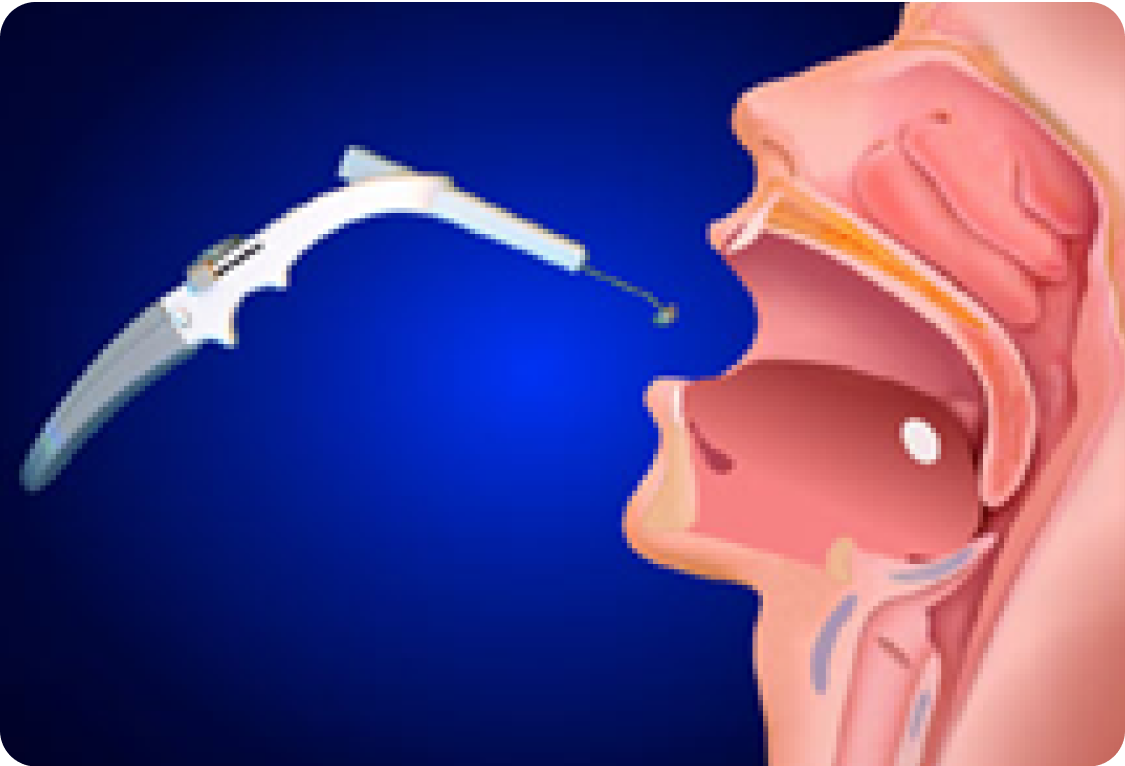
In severe cases the upper airway is very much narrowed and extra space need to be created and therefore requires volume reduction surgery. The surgery is aimed at creating more space in the Retro palatal (behind the soft palate) and retro lingual (behind the tongue) area. The collapsing area is diagnosis by looking with a nasopharyngoscope when sitting, lying down and also with quiet inspiration and expiration. This will give us an idea of collapsing sites in the airway. Some times sleep Nasendoscopy i.e. while patient is lightly sleep with intravenous medications, examination with nasopharyngoscope can replicate sleep conditions for us to ascertain areas of collapse. This will dictate which areas to treat i.e. soft palate or tongue base or both.
CT scan of the upper airway will also give valuable data as to the volume of tissue that needs removal. Some of the surgeries offered are listed here. For further information and details of surgery please talk to your surgeon.
Modified Uvuloplatal flap (modified UPPP)
Tongue reduction- with Somnoplasty
Tounge reduction- with Cobalation surgery
Palatal advancement- Tucker Woodson technique
Genial tubercle advancement
Hyoid suspension
Tracheotomy

Somnoplasty of the palate
Immediate post surgery
Palatal shortening at 6 weeks

Somnoplasty of the palate
Immediate post surgery
Palatal shortening at 6 weeks
Murali Mahadevan
Specialist ENT Surgeon
For all enquiries and appointments call (09) 925 4050
Suite A, Level 1, Kakariki Hospital
9 Marewa Road
Greenlane, Auckland 1051
Facsimile: (09) 925 4051
Only general information is provided on this web site and is not intended as advice or a consultation. Please read our full disclaimer.

If you're experiencing these symptoms, it's recommended to consult a healthcare professional for proper diagnosis and treatment.
FAQs
Snoring is caused by vibrations of soft tissues in the airway, while OSA occurs when the airway becomes partially or completely blocked during sleep.
Common symptoms include loud snoring, daytime fatigue, morning headaches, poor concentration, and restless sleep.
Risk factors include obesity, male gender, a large neck circumference, nasal obstruction, and anatomical factors like a recessed jaw.
Diagnosis is based on symptoms, physical examination, and sleep studies like polysomnography or overnight oximetry.
Treatment varies from lifestyle changes (weight loss, avoiding alcohol) to CPAP therapy, oral appliances, and surgical procedures for severe cases.
Yes, paediatric OSA is often caused by enlarged tonsils and adenoids, leading to snoring, hyperactivity, and difficulty concentrating.
Contact Us
Get in touch to book an appointment or inquire about our ENT services. Our team is here to assist you with expert care and guidance.
Ph: +64 9 925 4050
Fax: +64 9 925 4051
Dr Murali Mahadevan FRACS
Otolaryngology Associates Ltd
Suite A, Level 1, Kakariki Hospital
9 Marewa Road
Greenlane, Auckland 1051